The 10th Annual Conference of UPM Biomedicals, held on October 24, 2024, featured groundbreaking presentations from leading experts in drug discovery and cancer therapy. Experts discussed the transformative role of 3D cellular models, high-throughput screening, and advanced cell therapies in precision oncology. Andre Maia, PhD, of i3S, discussed the potential of 3D cellular models in advancing drug discovery. Timothy P. Spicer, PhD, from the UF Scripps Institute, explored the integration of automated high-throughput screening with 3D tumour models for precision oncology. Gerard Rubi Sans, PhD, of MiNK Therapeutics, presented their innovative iNKT cell therapy, MiNK-215, designed to remodel the tumour microenvironment and enhance anti-tumour immunity. These talks highlighted significant advancements shaping the future of biomedical research.
Advancements in 3D Cell Culture and High-Content Screening for Drug Discovery
Recent advancements in high-content screening (HCS) and 3D cell cultures are transforming drug discovery by providing more accurate models of human biology. Andre Maia, a biologist at the Institute for Research and Innovation in Health (i3S) in Portugal, is leading innovative research in this field.
High-Content Screening: A Powerful Tool in Drug Discovery
Since 2014, Maia has managed a platform for high-throughput and high-content screening, which uses advanced microscopy and image analysis to examine thousands of biological samples. This technology generates multi-parameter data that is crucial in understanding complex biological processes and contributes to early drug discovery. However, traditional 2D models often fail to replicate human biology accurately, leading to high failure rates in drug development, therefore better models are needed to emulate the human body.
3D Cell Cultures: Mimicking the Human Body
3D cell cultures offer a more realistic alternative, as they allow cells to interact in a way that better mirrors the human environment. Unlike 2D cultures, 3D models include oxygen gradients, multiple cell types, and extracellular matrices, providing a closer representation of how cells behave in the human body. These models also align with the 3Rs policy to reduce animal testing, and they support patient-derived models, target validation, and ex vivo clinical trials.
Challenges in 3D Model Adoption
Despite their promise, 3D models face challenges such as difficulties with automated liquid handling, interference in high-throughput and high-content screening often due to commonly used animal derived cell culture matrix properties, and imaging issues due to opacity. Overcoming these obstacles is essential for enhancing the scalability and reproducibility of 3D cell culture models used in drug discovery.

Innovative Projects and Collaborations
Exciting projects are demonstrating the potential of 3D models. For example, pediatric brain tumour organoids are being cultured without matrices, and microdevices are being developed to mimic blood flow in the human body. Additionally, research into organ-on-a-chip technologies and kidney organoids from liquid biopsies is furthering accurate organ modeling.
Through collaboration with UPM Biomedicals and using GrowDex hydrogels in their assays, Maia’s team is advancing the use of non-animal matrices that are compatible with automated liquid handling and robotics. As desired, the GrowDex hydrogels meet these criteria, including transparency for imaging and suitability for high-content screening.
The integration of 3D cell cultures and high-content screening is revolutionizing drug discovery, providing more reliable models that closely mimic human biology. While challenges remain, the collaboration between researchers and organizations like UPM Biomedicals is driving progress in developing more reproducible and representative drug testing methods.
Timothy Spicer: High-Throughput Screening and 3D Tumour Models in Precision Oncology
Timothy Spicer, a leader in high-throughput screening (HTS) and drug discovery at the University of Florida Scripps Institute, is making groundbreaking strides in cancer research, particularly in precision oncology. His expertise in HTS, coupled with his involvement in the Society for Lab Automation and Screening (SLAS), places him at the forefront of innovative cancer treatments.

High-Throughput Screening for Drug Discovery
Spicer’s team at the Scripps Institute uses advanced robotic platforms and automated systems to screen a library of over 3 million small molecules, processing up to 250,000 wells per day. Techniques high-content imaging enables efficient identification of potential drug candidates across various biological targets.
3D Tumour Models in Cancer Research
A key focus of Spicer’s research is the use of 3D tumour models, such as tumour organoids, which provide a more accurate representation of human cancer biology than traditional 2D cell cultures. These models, particularly for challenging cancers like glioblastoma, are derived from patient tumour cells and offer better predictions of treatment responses.
Drug-Gene Networking and Personalized Medicine
Spicer’s team integrates RNA sequencing with drug screening platforms using Drug-Gene networking analysis to identify personalized drug combinations. This approach has led to insights into the efficacy of drug combinations such as the treatment of a patient’s glioblastoma multiforme with Vemurafenib with Cobimetinib, contributing to more tailored treatment regimens.
Translating In Vitro Findings to Animal Models
To bridge in vitro findings to clinical applications, Spicer’s team tested these drug candidates in animal models. Their research has shown that the Vemurafenib + Cobimetinib drug combinations can significantly reduce tumour volume, especially in patient matched tumour implanted in the mouse brain, offering promise for treating complex cancers.
Overcoming the Blood-Brain Barrier
A major challenge in treating brain tumours is the blood-brain barrier (BBB). Spicer’s team collaborates with Marion Romano’s group by providing orthologous tumour samples, which are implanted into mice. Romano’s group utilizes laser interstitial thermal therapy (LITT) to temporarily open the blood-brain barrier (BBB), allowing access to the tumours for lavage and drug delivery. Pre-screened drug compounds from Spicer’s lab, are then tested for their ability to effectively treat the tumours. This collaborative workflow bridges in vitro genomic-driven drug profiling with in vivo validation, leveraging LITT to enhance therapeutic efficacy.

The Future of Cancer Treatment
Spicer’s research aims to develop scalable, cost-effective screening solutions for personalized cancer treatment. By incorporating machine learning and AI, the team hopes to optimize drug testing processes, making them faster and more efficient.
In conclusion, Spicer’s work is advancing the field of cancer research by moving towards more personalized, data-driven treatments. With continued progress in screening technologies and overcoming challenges like the blood-brain barrier, the future of cancer treatment holds great promise.
Advancing Cancer Therapy: Gerard Rubi Sans and MiNK Therapeutics' Breakthrough in 3D Tumour Modeling
Gerard Rubi Sans, scientist at MiNK Therapeutics, presented groundbreaking work in cell therapies for cancer. MiNK is pioneering treatments using innate natural killer T (iNKT) cells, which have shown promise in fighting solid tumours, including lung, colorectal, and liver cancers, without the need for patient lymphodepletion.
3D Models in Immunotherapy Development
Gerard highlighted the significance of 3D in vitro models in better mimicking human tumours and the tumour microenvironment (TME). His team used these models to assess MiNK-215, an engineered iNKT cell therapy targeting cancer-associated fibroblasts (CAFs), which are common in solid tumours and often suppress immune responses. By replicating the dense, immunosuppressive TME, the team could observe how MiNK-215 works in complex cancer environments.
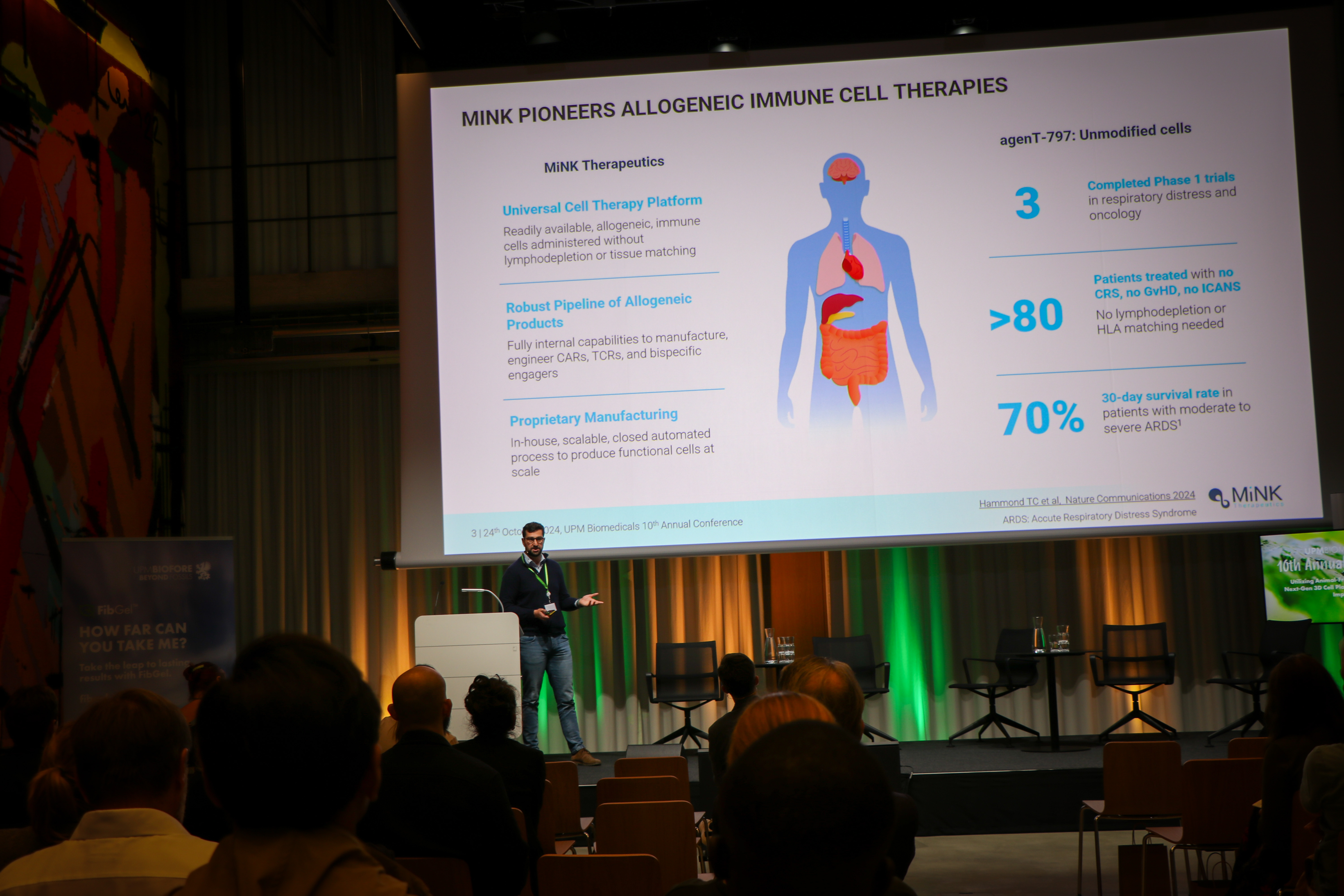
Preclinical and In Vivo Results
In preclinical studies, MiNK-215 demonstrated strong cytotoxic effects in 3D lung cancer and liver metastatic organoid models, targeting both tumour cells and CAFs. Combining MiNK-215 with T cells improved T cell recruitment and infiltration, targeting and killing the tumour. In vivo, MiNK-215 enhanced survival rates, reduced tumour size, and amplified T cell activity within the TME, showing great promise for future cancer treatments.
Future Prospects
MiNK Therapeutics is preparing to file for clinical trials in 2025. Gerard’s team is optimistic about the potential of MiNK-215 to revolutionize cancer therapy, especially when combined with other immune-oncology drugs. Their research also promises to reduce the need for animal studies, further advancing cancer immunotherapy.
MiNK Therapeutics, with the help of Gerard Rubi Sans, is pushing the frontiers of cancer treatment with innovative iNKT cell therapies and 3D tumour modelling. The development of MiNK-215 offers new hope for patients with difficult-to-treat cancers, marking a significant step forward in cancer care.

If you would like to watch the full sessions of the 10th Annual Conference, please click the link below: